Proteases are enzymes that break down proteins. Past studies have linked excessive production of human proteases with inflammation. However, the gut microbiome is an important source of proteases, which bacteria use to provide energy for themselves or as virulence mechanisms. Indeed, increased bacterial protease activity associated with gut microbiota changes was recently demonstrated in patients at risk for IBD before the onset of ulcerative colitis (UC).
A new study, conducted at the Farncombe Institute, in McMaster University, investigated whether bacterial proteolytic activity is also involved in Crohn’s disease (CD). The study, recently published in Gut Microbes, measured proteolytic activity in stool samples from patients with CD and then used these fecal microbial communities to colonize germ-free mice.
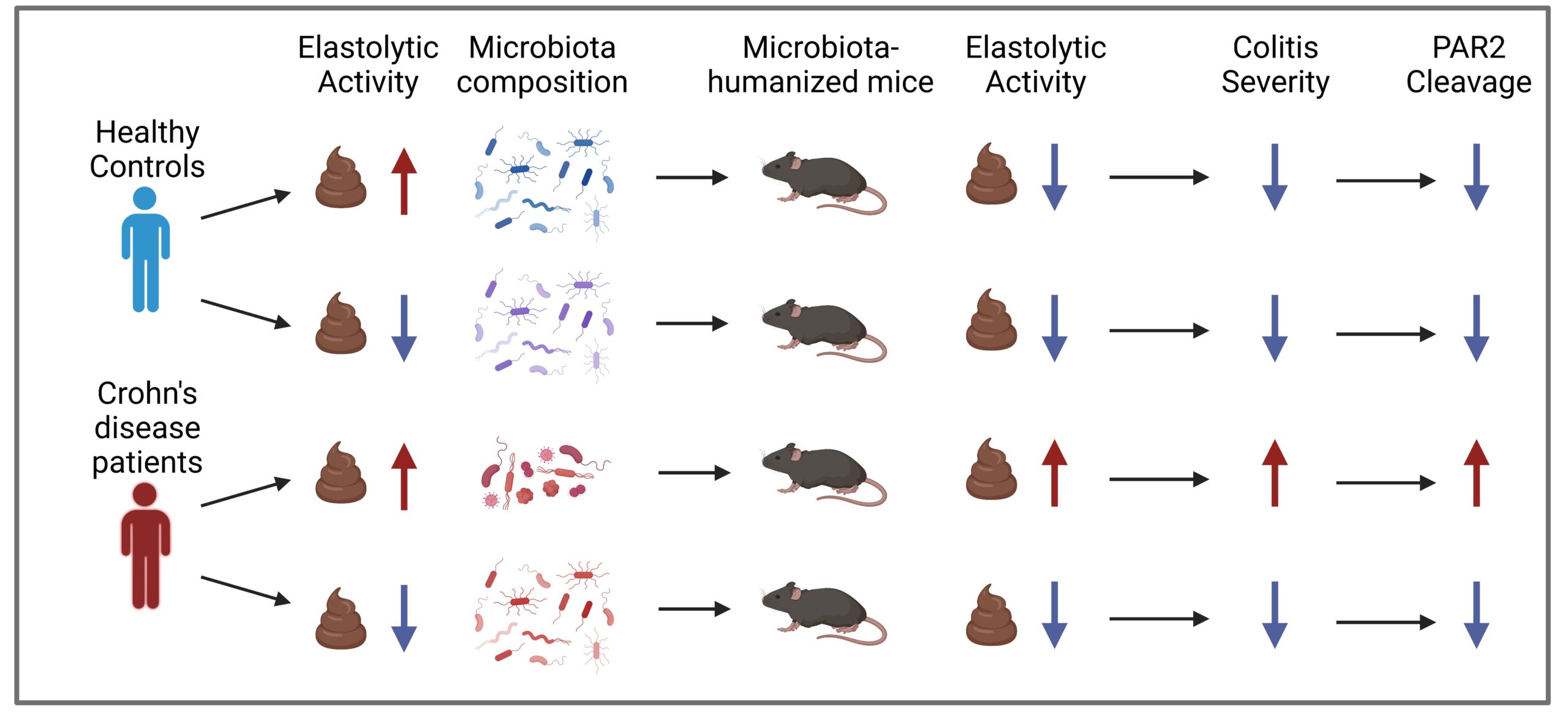
Mice colonized with stool that had high proteolytic activity developed high fecal proteolytic activity themselves, compared with mice colonized with low proteolytic microbiota or microbiota from healthy controls. The higher proteolytic activity was paralleled by increased proteinase activated receptor-2 (PAR2), but not PAR1, cleavage by the microbiota in vitro.
“Proteases with elastolytic activity, meaning they degrade elastin substrates, are pro-inflammatory. They cleave protease-activated receptor-2 (PAR2), expressed on the surface of many cell types including the gut epithelium and immune cells, activating downstream proinflammatory signalling pathways,” said first author Amber Hann, a PhD student in the Verdu lab at McMaster University.
Next researchers were interested in the microbiota differences observed between the fecal samples with low and high proteolytic activity. They found mice colonized with CD high proteolytic microbiota had an increased abundance of pathogenic taxa (e.g., Hungatella [formerly Clostridioides] hathewayi and Romboutsia ilealis) and a decreased abundance of beneficial taxa (e.g., Akkermansia muciniphila, Alistipes putredinis, and Ruminococcus bromii).
Unsurprisingly, the two CD microbiotas also had distinct predicted functional profiles. Several serine proteases were differentially expressed. Specifically, the protease K04772 was observed to be increased in the high proteolytic CD microbiota. Using analyses of functional predictions of microbial communities, the researchers demonstrated that mRNA transcripts of the protease K04772 positively correlated with increased mRNA transcripts of H. hathewayi. Thus, they concluded one source of the proinflammatory protease activity seen in this CD cohort studied is from H. hathewayi.
Investigators then colonized additional germ-free mice with high or low proteolytic CD microbiota and subjected them to intestinal injury. Having high proteolytic CD microbiota made the mice more susceptible to intestinal injury and colitis. To investigate mechanisms, germ-free mice lacking Nod2 (a common polymorphism in CD involved in bacterial sensing; Nod2-/-) and mice lacking cleavable PAR2 were colonized with high proteolytic CD microbiota. Nod2-/-developed severe colitis, but mice lacking cleavable PAR2 were protected from colitis, indicating this is a key event by which proteolytic CD microbiota mediates inflammation.
Overall studies that support a role of bacterial protease activity in the pathogenesis of CD and UC are mounting. “Proteases are important for bacteria to survive but can also drive inflammation, especially if present in high abundance” explains Amber, who is currently investigating the factors that drive the high bacterial protease activity, so that this proinflammatory activity of the microbiome can be prevented.
Although these findings cannot rule out the involvement of host proteolytic enzymes, they support that specific microbial proteolytic signatures can be targeted for interventions in patients with CD, preferably at an early stage of the disease. Establishing a role for microbial proteolytic activity in IBD could lead the development of anti-proteolytic therapies directed at the bacterial taxa involved or the factors that drive this proinflammatory activity.
Adapted from: Galipeau HJ, Caminero A, Turpin W, Bermudez-Brito M, et al. Gastroenterology 2021.
References:
Galipeau, H. J. et al. Novel Fecal Biomarkers That Precede Clinical Diagnosis of Ulcerative Colitis. Gastroenterology 160, 1532–1545 (2021).
Santiago, A. & Hann, A. et al. Crohn’s disease proteolytic microbiota enhances inflammation through PAR2 pathway in gnotobiotic mice. Gut Microbes 15, 2205425 (2023).