Deep inside your small intestine is a region that’s critical in the body’s immune system: the gut-associated lymphoid tissue (GALT). At this site, your body’s cells interact with both microbes and immune cells, and the results of their interactions decide whether you will tolerate the things encountered in the gut—whether a particular food molecule or a foreign microbe—or alternatively, whether your body will mount an immune system attack. And new research shows commensal gut microbes in the GALT help make an immune cell that enables its host to function normally by tolerating harmless substances from the outside environment.
In the study published in Science, the researchers from Washington University School of Medicine in St. Louis (USA) wanted to investigate the making of a unique immune cell: a type of T cell called a ‘double-positive intraepithelial lymphocyte’, or DP IEL for short. These cells exist in the small intestine and normally help the body to discriminate what is “self” and what is “non-self”, and to tolerate dietary substances and other molecules from outside the body, dampening inflammatory responses.
Body cells interact with bacteria and immune cells at the same time in the GALT
Scientists have found that DP IELs are absent in germ-free mice, which live their lives in a sterile environment without exposure to any bacteria. So do gut microbes play a role in making these tolerance-promoting immune cells? The researchers wanted to find out.
They began a process of colonizing groups of germ-free mice with various bacteria: strains of Lactobacillus and Bacteroides. Sure enough, one kind of bacteria in particular led to the production of DP IELs in the mice: Lactobacillus reuteri. And interestingly, although other species of bacteria did not induce DP IELs by themselves, the effect of L. reuteri was enhanced by adding other species into the mix.
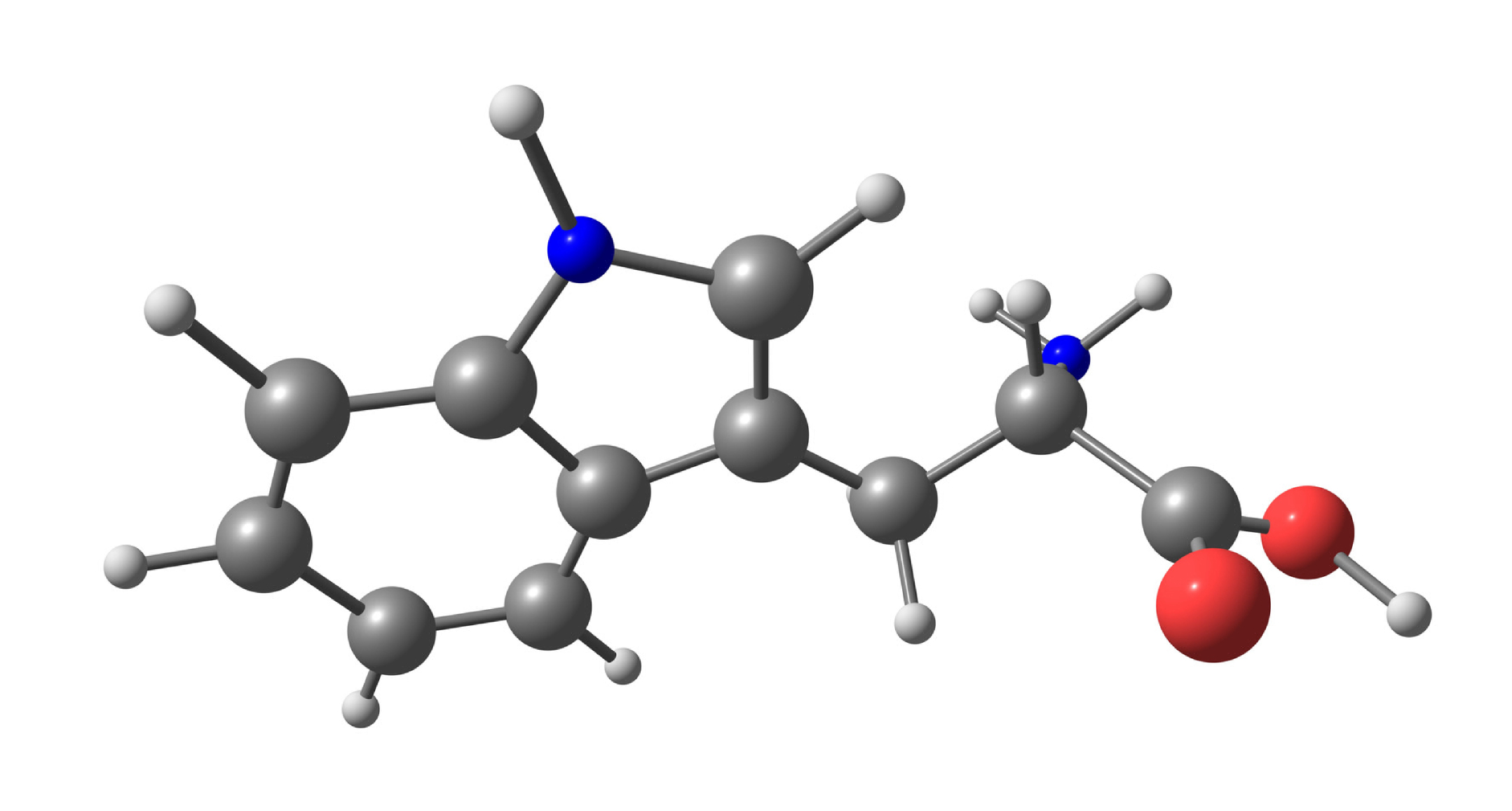
The scientists also found a certain component of the mouse diets was necessary for kick-starting the production of these DP IELs. It was L-tryptophan—an essential amino acid that acts as one of the building blocks of proteins. (Tryptophan is a normal part of both mouse and human diets, and is present in items like soy beans, milk, nuts, eggs, and yogurt.) The active ingredient for DP IEL production appeared to be a byproduct of tryptophan metabolism called indole-3-lactic acid. More DP IELs were found in the mice fed a diet rich in L-tryptophan. Putting everything together, the researchers concluded that in the mice they studied, L. reuteri co-operated with dietary tryptophan to make the important DP IEL cells.
Tolerance of any elements in the intestine depends on the relationship between the body’s cells and both bacteria and immune cells
The idea that maturation of the DP IEL anti-inflammatory immune cells depends on L. reuteri and its tryptophan metabolites is just the latest example of diet-microbe teamwork as an important factor in immune system processes.
It’s not yet known whether the exact same process occurs in humans. But “…the development of these cells is probably something we want to encourage since these cells control inflammation on the inner surface of the intestines,” says first author Luisa Cervantes-Barragan of Washington University School of Medicine. “Potentially, high levels of tryptophan in the presence of L. reuteri may induce expansion of this population.” One day, say the authors, the research may lead to new interventions for inflammation-related diseases like inflammatory bowel disease that may be modifiable by DP IELs.
Reference:
Cervantes-Barragan L, Chai JN, Tianero MD, DiLuccia B, Ahern PP, Merriman J, Cortez VS, Caparon MG, Donia MS, Gilfillan S, Cella M, Gordon JI, Hsieh C-S, Colonna M. Lactobacillus reuteri induces gut intraepithelial CD4 CD8 alpha alpha T cells. Science. 2017; 357(6353): 806-810. doi: 10.1126/science.aah5825.