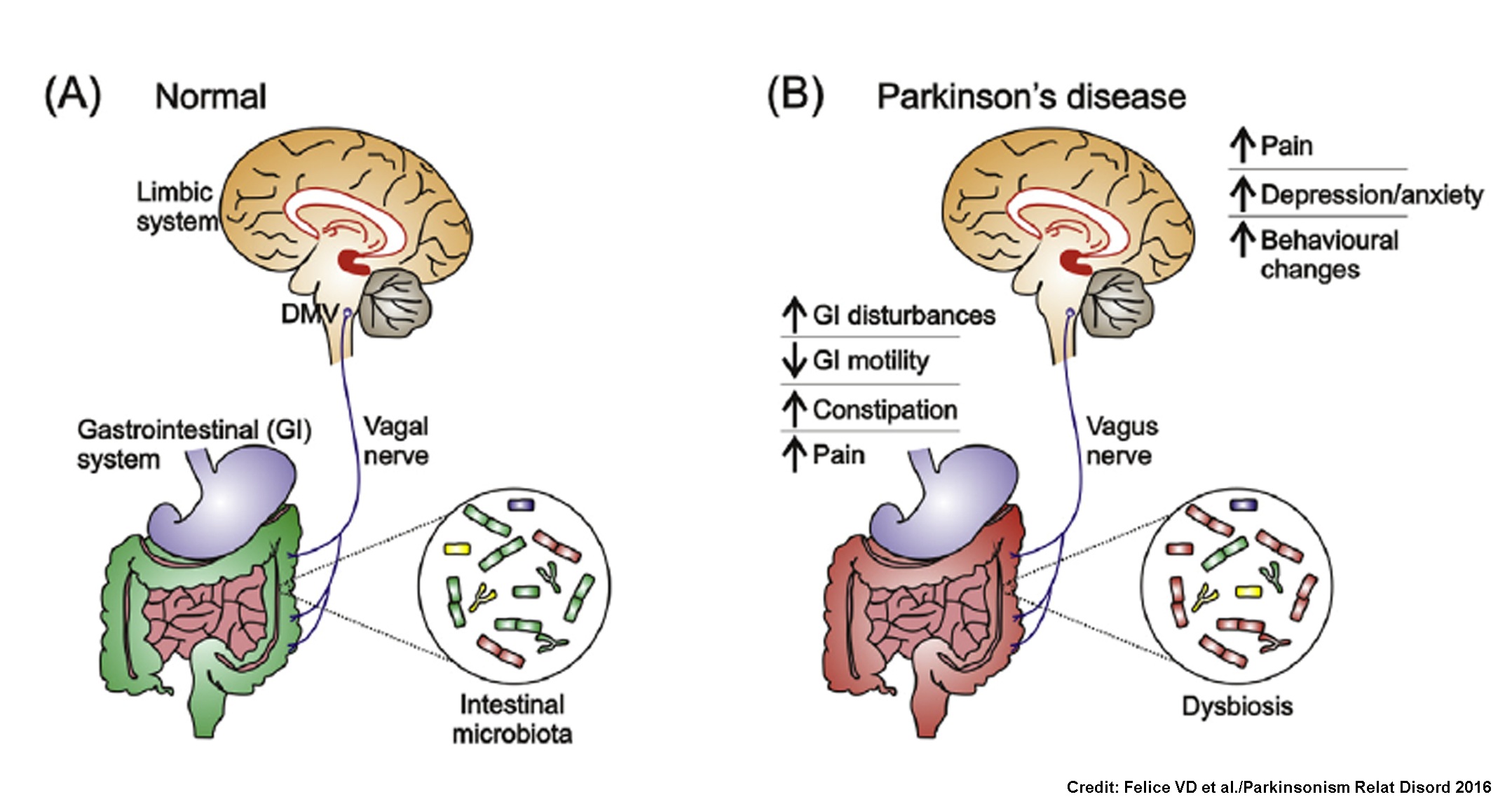
Recent research has given important insights into the role of gut microbiota alterations in Parkinson’s disease (PD). Although motor deficits (including tremor, bradykinesia and rigidity) are the cardinal symptoms of PD, non-motor symptoms (NMS) (constipation, gastrointestinal disturbances, sleep disturbances and sensory alterations, among others) are also apparent and affect PD patients’ quality of life more negatively than the motor symptoms. NMS symptoms are often evident before the classic motor symptoms and a recent hypothesis suggests they may be linked to a dysfunction in the communication between gut and brain.
Until now, three case-control studies have assessed gut microbiota in PD: a Finnish study, an American study, and a Japanese study. Although all of them found significant differences between gut microbiota of PD patients and controls, the results differed in terms of differentially abundant taxa and associations of gut microbiota with clinical variables. A recent review gives an in-depth comparison of the three studies (demographic characteristics of both PD patients and controls, antibiotic and probiotic exposure, methodology, relevant findings related to microbiota composition, strengths and limitations). The differences in results may be partially explained by methodological differences between studies regarding geographical regions, ethnicities, disease stages, selection criteria of participants, statistics, and confounder control. Therefore, such aspects should be taken into account in further studies aimed at establishing the exact nature of the changes involved in alterations of gut microbiota in PD.
Taking things one step further, a recent study, led by Dr. Karl-Herbert Schäfer from the Department of Biotechnology at the University of Applied Sciences Kaiserslautern in Zweibrücken (Germany), has found that gut microbiota dysbiosis in PD may be associated with a shift in short-chain fatty acids (SCFAs), one of the main metabolic products of the gut microbiota.
The researchers analysed SCFA concentrations and gut microbiota composition in faecal samples of 34 PD patients (mean age 67.7 years) and 34 age-matched controls (mean age 64.6 years). A third group of young controls (mean age 33.3 years) was also included to identify age-related alterations.
The bacterial phylum Bacteroidetes and its family Prevotellaceae were significantly reduced in faecal samples of PD patients. By contrast, Firmicutes was the most abundant phylum and showed a similar relative abundance in all groups. Faecalibacterium prausnitzii, Lactobacillaceae and Enterococcaceae (phylum Firmicutes) were significantly reduced in the samples of PD patients compared to age-matched controls. Besides this, Enterobacteriaceae (phylum Proteobacteria) and Bifidobacterium were more abundant in individuals with PD compared to age-matched controls.
Faecal SCFA concentrations (acetate, propionate and butyrate) were significantly reduced in PD patients compared to controls. Although a causal relationship cannot be inferred yet, the researchers hypothesized that reduced concentrations of butyrate in the faeces of PD patients may be associated with altered SCFA effects on the enteric nervous system, perhaps contributing to gastrointestinal dysmotility, a frequent NMS in PD.
On the whole, alterations of gut microbiota are present in Parkinson’s disease, though it is unclear whether specific features gut microbiota composition are relevant to disease onset and progression. The exact mechanisms involved and the role of gut microbiota and microbial products in the development of PD and PD-associated NMS are not established yet; future larger studies in this field would add new insights.
References:
Felice VD, Quigley EM, Sullivan AM, O’Keeffe GW, O’Mahony SM. Microbiota-gut-brain signalling in Parkinson’s disease: Implications for non-motor symptoms. Parkinsonism Relat Disord. 2016; 27:1-8. doi: 10.1016/j.parkreldis.2016.03.012.
Scheperjans F. Gut microbiota, 1013 new pieces in the Parkinson’s disease puzzle. Curr Opin Neurol. 2016; 29(6):773-80. doi: 10.1097/WCO.0000000000000389.
Unger MM, Spiegel J, Dillmann KU, et al. Short chain fatty acids and gut microbiota differ between patients with Parkinson’s disease and age-matched controls. Parkinsonism Relat Disord. 2016; 32:66-72. doi: 10.1016/j.parkreldis.2016.08.019.