The fact some people respond to a drug treatment while for others the same treatment is totally ineffective may depend on our gut microbiota. In other words, after a drug is administered orally, it could either be absorbed into the bloodstream and metabolized by the liver, or it remains in the intestine where it can be metabolized by the gut microbiota.
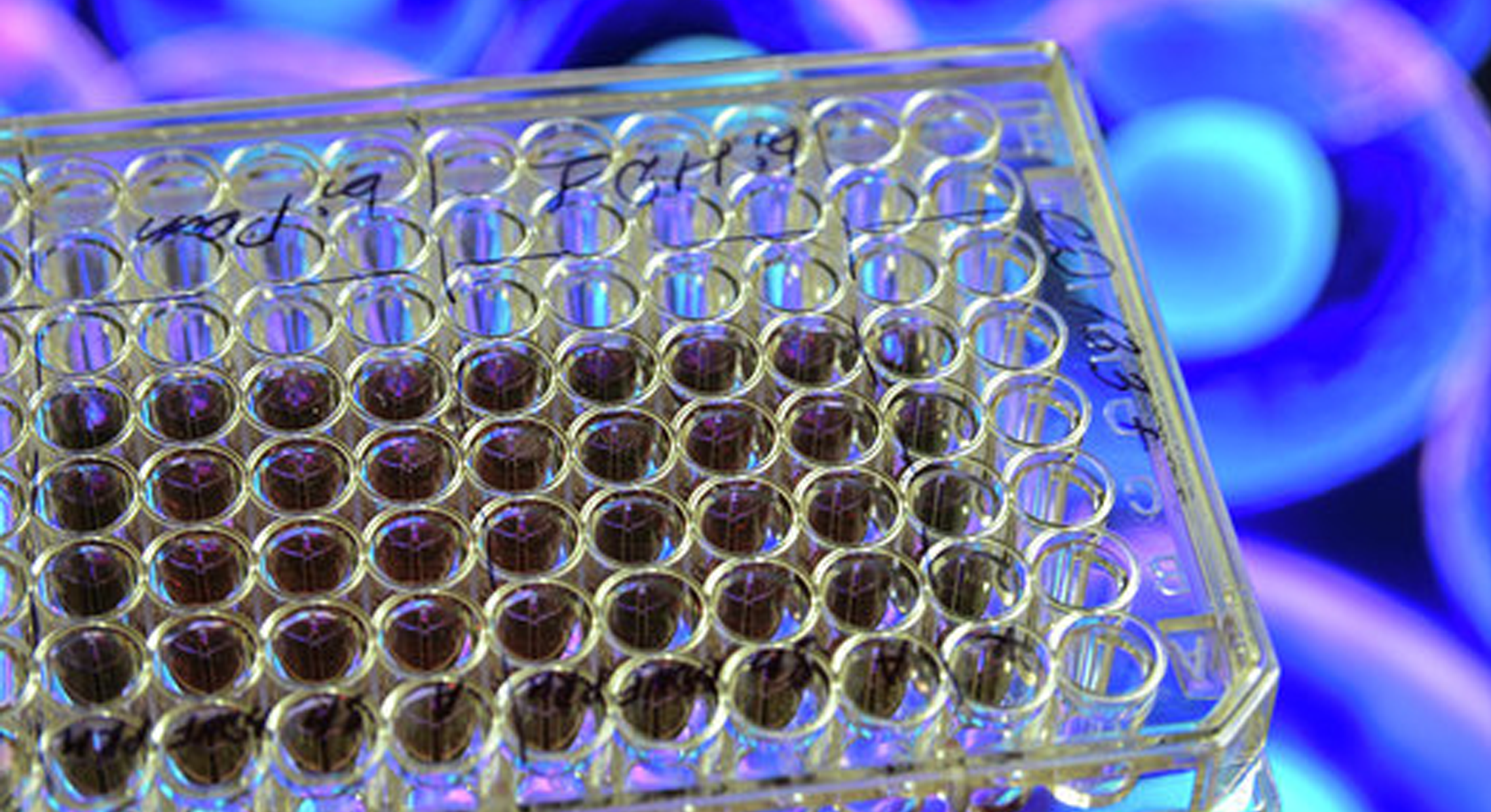
In the light of the fact that the way drugs are metabolized by gut bacteria remains largely underexplored, Zimmermann and colleagues have tested in vitro the ability of 76 human gut bacterial strains to metabolize 271 commonly used drugs with diverse structures and functions.
Using in vitro tests, the authors assessed how the metabolism of 271 drugs (excluding antibiotics) by 76 bacterial isolates from the human gut—including species belonging to the main bacterial taxonomic groups—occurs. Drugs were chosen according to the diversity of their molecular structures and therapeutic effects.
Of the 271 drugs studied, 176 (65%) were metabolized by at least one bacterial strain, which resulted in a more than 20% reduction in the level of active drug molecules.
Each bacterial strain was capable of metabolizing a number of the drugs, ranging from 11 to 95. It was also possible to differentiate groups of drugs that are metabolized differently by gut bacteria depending on the compounds’ chemical structure.
Mass spectrometry analysis revealed that the 176 metabolized drugs led to 868 metabolites, which indicates that gut bacteria produce more than one metabolite per drug molecule. Specifically, the chemical transformations involving the gut microbiota included acetylations, oxidations and reductions.
In a second step, the authors wanted to figure out which bacterial enzymes were responsible for drug metabolism. To do that, they explored the contribution of Bacteroides thetaiotaomicron—previously shown to be involved in metabolizing 46 of the drugs tested—in metabolizing the antihypertensive drug diltiazem.
Isolated sections of the B. thetaiotaomicron genome were inserted into plasmids, which were subsequently inserted into Escherichia coli to explore the final phenotype. When E. coli were exposed to diltiazem, a subset of the bacteria metabolized the drug, whereas some of the bacteria did not.
The E. coli bacteria that metabolized diltiazem helped researchers identify the codifying gene bt4096 responsible for its metabolism. Taking a similar approach, they also identified genes involved in metabolizing 18 drugs using B. thetaiotaomicron.
On the whole, this study has looked in detail at how widespread drug metabolism by the gut microbiota occurs. As the researchers tested a wide range of drugs, these findings highlight the microbiota’s contribution to activating or deactivating drugs.
According to the authors, the genetic make-up of patients’ gut microbiota could, one day, help doctors predict which drug might be best suited for each individual. In addition, knowing what effects each drug causes in the microbiota could help with developing more effective drugs.
The discovery also opens the door to modulating the gut microbiota in order to increase the efficacy of a drug or reduce the side effects it causes. For instance, diet could also affect the efficiency of drugs by altering the microbiota, thus highlighting the complexity of the field of personalized medicine.
Reference:
Zimmermann M, Zimmermann-Kogadeeva M, Wegmann R, Goodman AL. Mapping human microbiome drug metabolism by gut bacteria and their genes. Nature. 2019; 570(7762):462-7. doi: 10.1038/s41586-019-1291-3.