Although the human gut microbiome is a source of antibiotic resistance genes (ARGs), until now, the intestinal resistome has not been extensively characterized. Challenges therefore remain, and they include figuring out the gut microbiota’s contribution to the total pool of known ARGs and identifying ARGs in metagenomic data, given that they show distant homologies with known genes in databases.
Researchers from MetaGenópolis, Paris Diderot University, Institut Pasteur, the Spanish National Research Council, the Ramón y Cajal Health Research Institute, CIBER Epidemiology and Public Health, Beaujon Hospital, Bichat-Claude Bernard Hospital, University Medical Center Utrecht, the University of Birmingham and King’s College have developed a new bioinformatics gene function prediction method by characterizing the structure proteins of the human gut resistome.
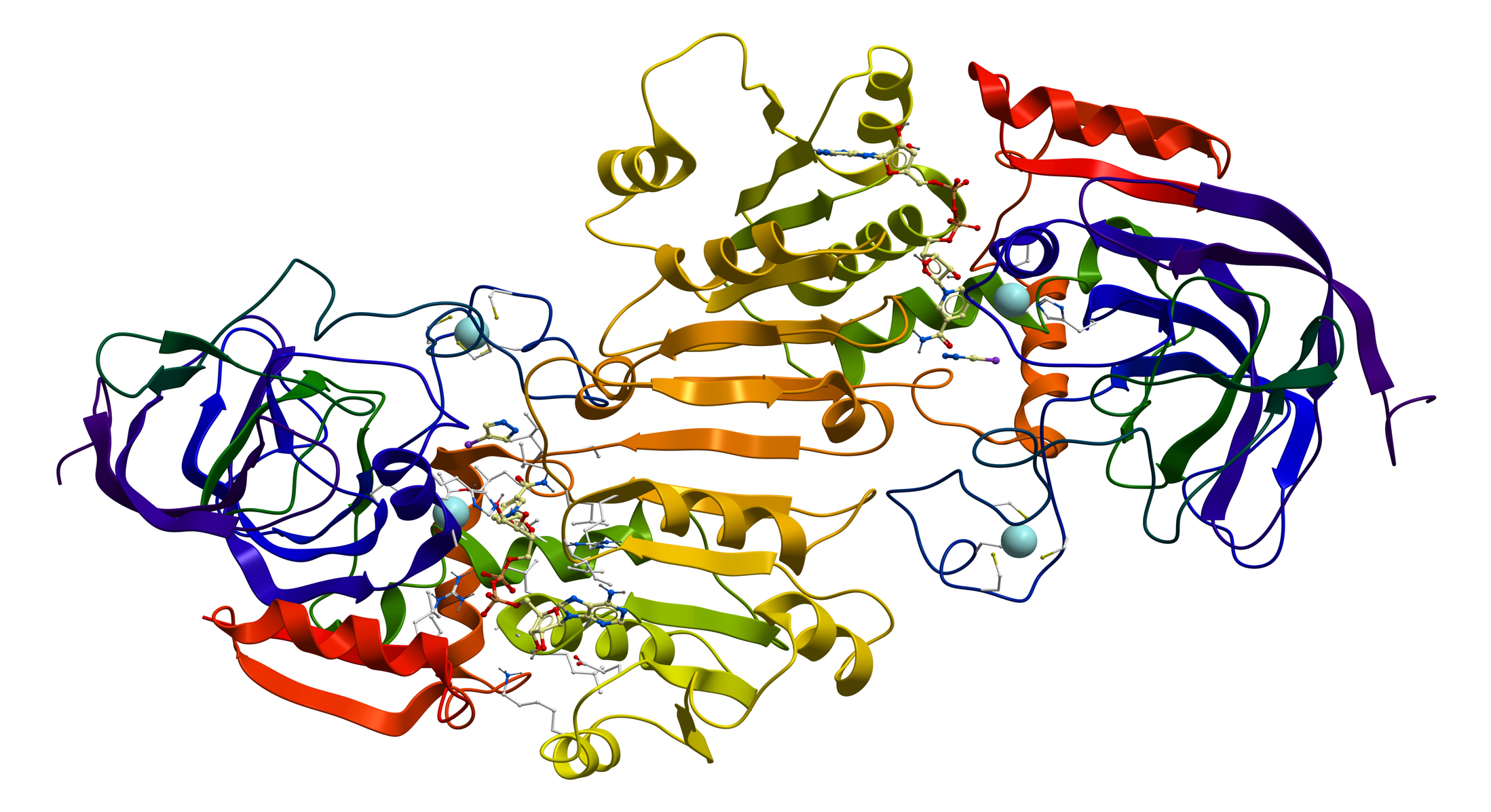
In their new paper, the scientists developed and validated a new method for predicting ARGs in the intestinal microbiota based on the three-dimensional (3D) structure of proteins codified by ARGs.
The method, called pairwise comparative modelling, allowed for predicting the 3D position of every atom from unknown proteins based on the known structure of a similar protein previously obtained through crystallography. This approach was based on the fact that: 1) The structure of a protein is uniquely determined by its amino acid sequence; and 2) Protein structure is more stable and changes more slowly than the associated sequence.
Etienne Ruppé, first author of the study, emphasizes that, beyond its use for exploring ARGs, homology comparative modelling helps predict proteins that may be a distant relation of known proteins.
After validating the method, it was applied to the 3.9 million MetaHIT gene catalogue built from the metagenomic sequencing of 396 subjects from Denmark and Spain. Consequently, the method predicted the presence of 6,095 ARGs in the human gut—involved in conferring resistance to b-lactams, aminoglycosides, tetracyclines, macrolides, quinolones, sulfonamides, trimethoprim, fosfomycin and glycopeptides—with each of us carrying an average of 1,300 ARGs.
The majority of predicted ARGs were distantly related to known ARGs and most of them were not found either on mobile genetic elements or in pathogenic bacteria. Contrary to a previous hypothesis, these data did not support the idea that ARGs are transferred between species.
Furthermore, exposure to antibiotics affected the content of the ARGs. The number of gut microbial genes (gut bacterial richness) was positively associated with an abundance of ARGs among hospitalized individuals who did not receive antibiotics. Short, high-dose exposure to antibiotics altered the composition of the intestinal microbiota and decreased gene richness, whereas the relative abundance of ARGs remained stable. However, chronic exposure to antibiotics was associated with an increased abundance of certain ARGs in parallel with a fall in gene richness and changes in the gut microbiota at the phylum level.
Meanwhile, the composition of the participants’ resistome allowed researchers to identify six groups of individuals (named ‘resistotypes’, a specific microbiota profile enriched with ARGs). Notably, those resistotypes were related to previously described enterotypes.
With this new study, researchers have, for the first time, carried out an in-depth characterization of ARGs in the gut microbiota through a new method based on the 3D structure of the proteins they encode. Contrary to previous research, this supports the idea that most gut microbiota-related ARGs are intrinsic to the gut microbial species, rather than being transferred with bacterial pathogens.
Reference:
Ruppé E, Ghozlane A, Tap J, et al. Prediction of the intestinal resistome by a three-dimensional structure-based method. Nat Microbiol. 2018. doi: 10.1038/s41564-018-0292-6.