On June 27th is the World Microbiome Day; on this occasion GMFH editors took time to interview Dr. Rob Knight, the founding Director of the Center for Microbiome Innovation and Professor of Pediatrics at the University of California San Diego, about some key aspects of gut microbiota and how microbes could help mitigate the raise of antibiotic resistance.
Factors such as diet, antibiotics and geography can influence the microbial make-up of the gut
Major observations that from different studies and science projects, have showed that lifestyle and diet affect the diversity of the human gut microbiome. For instance, the number of plant types in a person’s diet has the strongest effect on the diversity of his or her gut microbiome. “The difference between people who eat just a few types of plants per week versus those who eat over 30 types was a stronger effect than recent antibiotic use,” says Rob Knight.
“We plan to explore other environments across the globe and beyond the human gastrointestinal tract,” says Rob Knight
“Fortunately we can expect to collect more data through the American Gut Project (AGP), now part of The Microsetta* Initiative (TMI),” Rob Knight explains. To date, over 21,000 people are part of the project, across more than 40 countries. Besides examining the gut microbiome, scientists collected dietary habits (micro- and macro-nutrients), anthropometric measures (height, weight), lifestyle and disease information of participants through validated questionnaires.
“We plan to explore other environments across the Globe and beyond the human gastrointestinal tract due to the crucial contribution of microbes for achieving an environmentally sustainable future, by including a more global population and improve the collection of the participants’ diet habits to increase the knowledge of the microbiome’s impact on human health. The ultimate goal is to develop nutritional tailored solutions for a healthy gut and microbiota,” Knight concludes.
Understanding what a healthy microbiome remains a challenge
One of the main challenges in microbiome research is understanding what a healthy microbiome is. According to Rob Knight, “the definition of a healthy gut microbiome may be context-dependent and highly personalized (e.g., for particular age ranges, populations, etc.). As a result, we can’t define what a healthy microbiome is based on whether specific organisms are present. In fact, we can’t even do the opposite: an unhealthy microbiome cannot be defined by the presence of pathogenic bacteria because it is normal to observe organisms thought of as pathogens, such as Clostridium difficile, in healthy individuals”.

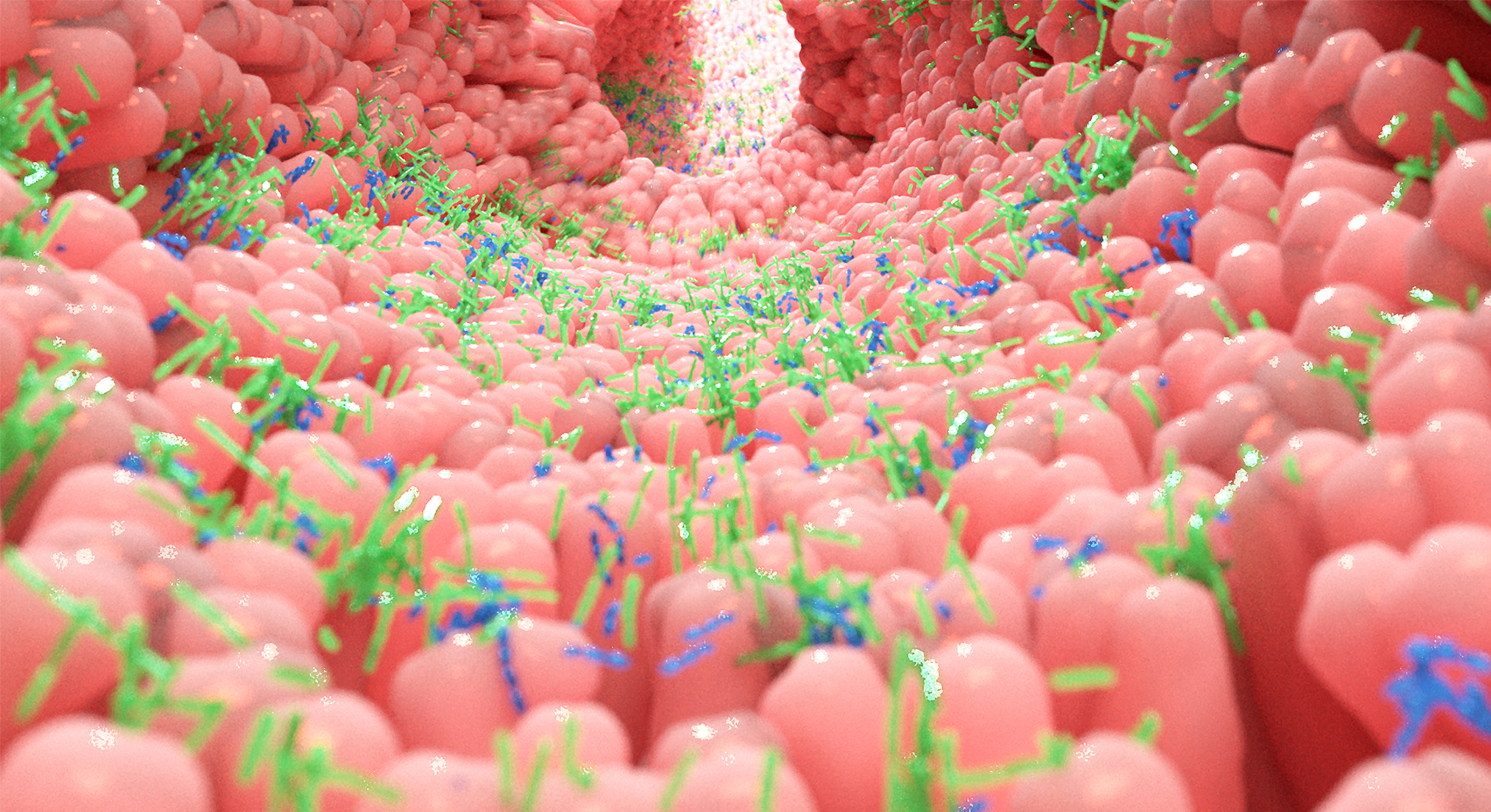
Photo by Casey A. Cass/University of Colorado
Diet, probiotics and phages may help battle antibiotic resistance
Focusing on the theme of the 2019 World Microbiome Day, and regarding the impact of diet in helping to limit the rise in antibiotic resistance, Rob Knight clarified that it’s a promising field but still in its infancy. For instance, antibiotics have been detected in fecal samples in individuals who self-reported no consumption of antibiotics in the past year!
Interestingly, individuals who ate more than 30 different plants per week also had fewer antibiotic resistance genes in their gut microbiomes than people who ate 10 or fewer plants. Scientists should explore why this occurs and the long-term impact of antibiotic consumption on the gut microbiome.
According to Rob Knight, “The definition of a healthy gut microbiome may be context-dependent and highly personalized.”
Beyond diet, regular consumption of probiotics might also help mitigate the rise of antibiotic resistance. A recent review of multiple studies showed that infants and children who consumed probiotics to reduce the appearance and duration of acute respiratory and digestive tract infections have a lower risk of being prescribed antibiotics.
On how the gut microbiota can be manipulated to reduce bacterial resistance to antibiotics, Prof. Steffanie Strathdee from UC San Diego is pioneering phage therapies (that is, the use of viruses that attack bacteria to treat infections) to combat antibiotic resistant bacteria associated with life threatening diseases. Phages are thus another potential tool that may contribute to reducing the current burden in antibiotic resistance.
*: The Microsetta Initiative has three main goals. 1/, to allow anyone in the world to engage in microbiome research, 2/ to ethically gather information about general health status, disease history, lifestyle and diet of participants to better understand human microbiomes between populations, and 3/ to generate high-quality data about the unique microbial communities that inhabit our bodies that will be available for ongoing reuse by anyone.