Our gut microbiota’s composition and metabolic activity is behind the close relationship between what we eat and our gut health and wellbeing.
You have probably experienced gastrointestinal symptoms related to food intake, which can be aggravated by certain foods or food groups. And you’re not alone in that. As increasingly more people are affected by digestive disorders that affect their quality of life, it’s no surprise that different diets for improving gut health are being promoted worldwide in blogs and cookbooks.
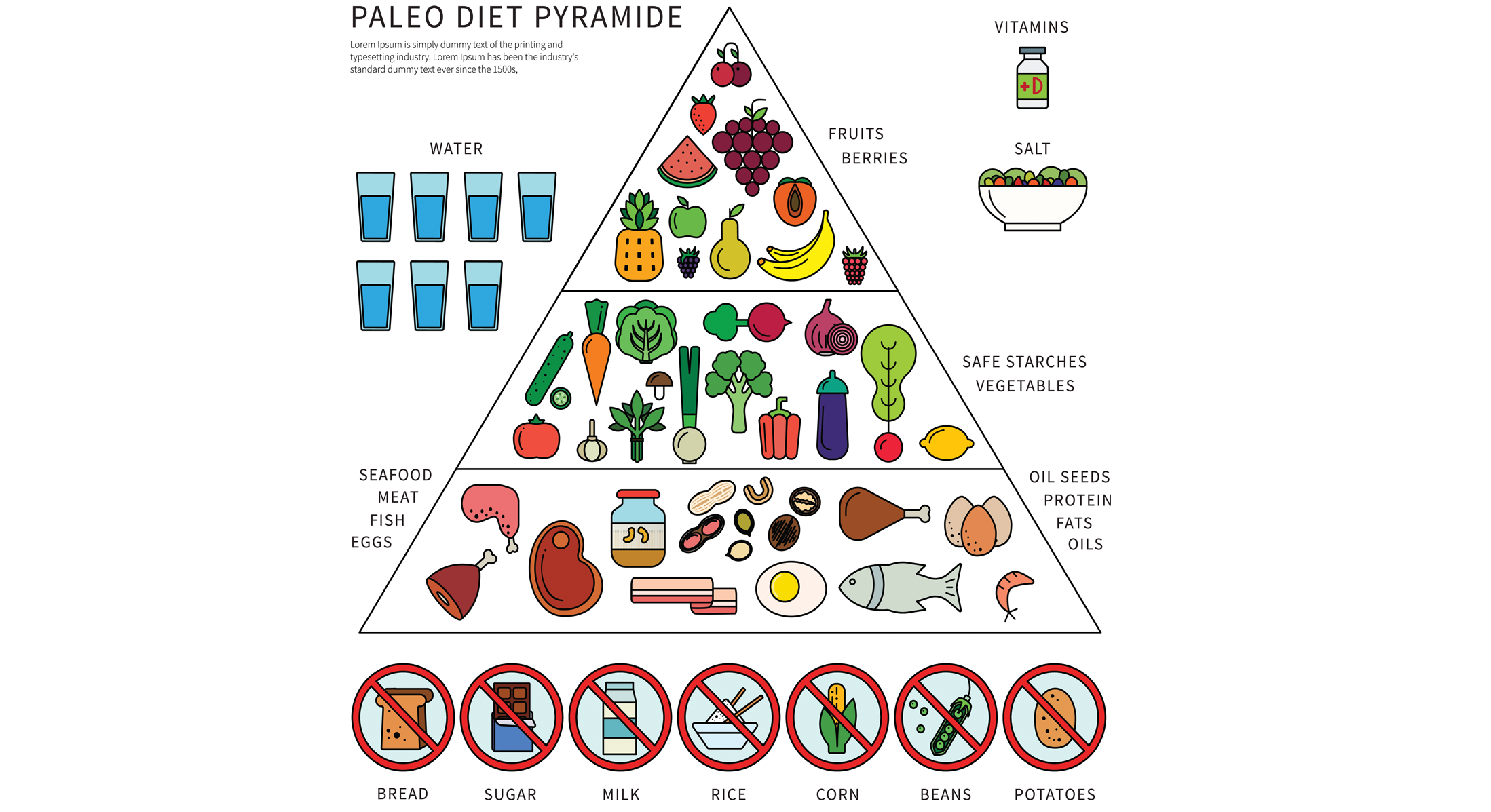
Among these trendy diets, the Paleolithic (paleo) diet, which excludes grains, dairy and legumes, occupies an important position. Despite its popularity, however, its health benefits and long-term side effects have yet to be documented.
Angela Genoni from the Edith Cowan University in Australia and colleagues have found that following a paleo diet for more than 1 year is associated with unfavorable changes in gut microbiota composition and increased levels of trimethylamine N-oxide (TMAO), an organic compound involved in the development of cardiovascular disease.
Compared with individuals who followed a balanced diet that included grains, legumes and dairy, a negative impact on the gut microbiota was observed among those consuming a paleo diet, as seen by the:
- Higher abundance of gut microbes such as Hungatella, which produce greater amounts of TMAO; and
- Decreased levels of beneficial gut bacteria that ferment dietary fiber, such as Bifidobacterium and Roseburia.
Those changes in gut microbiota were accompanied by high levels of TMAO—a compound involved in narrowing or obstructing the arteries—in the blood, especially in individuals who followed a strict paleo diet.
These findings highlight that excluding certain foods or food groups can deprive your gut microbiota of the ability to work properly, with consequences that go beyond your gut
The impact of the paleo diet on participants’ health does not end there. Participants consuming a paleo diet had a decreased intake of resistant starch, which is broken down by the gut microbiota, leading to the production of chemicals that are known to be good for our health. In addition, the higher levels of blood TMAO levels were linked to low intake of whole grains. That’s why the authors conclude higher whole grain consumption could be beneficial for those on a paleo diet.
These findings highlight that excluding certain foods or food groups can deprive your gut microbiota of the ability to work properly, with consequences that go beyond your gut. For instance, a lack of grains in a person’s diet can affect their heart health by increasing their levels of TMAO.
Maintaining a varied and balanced diet may help improve gut and metabolic health via the gut microbiota.
If you decide to make changes to your diet, the best advice is to avoid any radical action. Consulting a health professional is strongly recommended, with dietitians able to advise you on food choices for helping you improve your gut health and general wellbeing.
References:
Böhn L, Störsrud S, Törnblom H, Bengtsson U, Simrén M. Self-reported food-related gastrointestinal symptoms in IBS are common and associated with more severe symptoms and reduced quality of life. Am J Gastroenterol. 2013; 108(5):634-41. doi: 10.1038/ajg.2013.105.
Genoni A, Christophersen CT, Lo J, et al. Long-term Paleolithic diet is associated with lower resistant starch intake, different gut microbiota composition and increased serum TMAO concentrations. Eur J Nutr. 2019. doi: 10.1007/s00394-019-02036-y.